I've
written about the financial difficulties leading to the closure of Quincy Medical Center and have suggested that these almost inevitably resulted from the business model employed by the private equity firm that owns this hospital system. But are there other somewhat hidden consequences of this style of ownership? One worth reviewing might be the system's commitment to residency training programs.
St. Elizabeth's Medical Center is the major training hospital within the Steward Health Care System. How is it doing with regard to the long-standing and clinically important graduate medical education program that resides there?
Not so good.
The ACGME is the governing body that accredits residency programs. It has
a public website on which the status of each program is listed. As we go through the site, we see the following programmatic problems at St. Elizabeth's in three of its largest training programs. (The fourth, Anesthesiology, is currently accredited but up for renewal soon.)
Surgery
Internal Medicine
Psychiatry
Getting a warning or probationary designation is a very big
deal. For example, of the
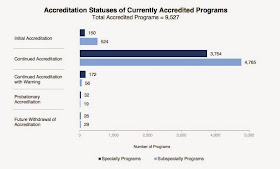
9,527 programs that were ACGME accredited in 2013-2014, only 279 programs (under 3%) received such designations. Here's the chart:
A warning is serious, but probationary status is applied when the ACGME concludes, following a site visit and review, that a program or
sponsoring institution has failed to demonstrate substantial compliance
with ACGME requirements.
What's behind the St. Elizabeth situation? While the details behind these designations are not published, in general, the largest number of such citations come from persistent violations of the ACGME duty hours requirements. Recall that, several years ago, the ACGME imposed
strict limits on the number of hours per week that residents were permitted to work. These rules came about from Congressional pressure and an acknowledgement that it was not healthy for the residents, patients, and members of the public for trainees to get
too little sleep (resulting in "impaired neurocognitive performance, including reduced memory
consolidation, and deterioration of waking performance marked by
increased rates of attentional failures.")
I have a hypothesis that when a hospital like St. Elizabeth's suffers from financial distress, there is an inclination to use residents as low-cost labor (relative to nurse practitioners and physician assistants) and assign them to extra hours of work in taking care of patients. I'd be happy to have this hypothesis disproved, but that would require disclosure by St. Elizabeth's of the reasons for the warning and probationary ACGME designations. The hospital is very unlikely to provide that to me!
But is there any inclination on the part of the Attorney General, the state official with
authority to monitor the performance of the Steward Health system, to look into this matter? If residents are, in fact, violating duty hours, there is the potential for harm to the public. If residents are being assigned to cover the work that would otherwise go to paid staff, is that consistent with the employment promises made during the take-over of the system from its previous owners?
(There is also another possible reason for poor reports from the ACGME--a lack of training opportunities. For example, if the volume of patients is too low, surgical residents don't get enough cases on which to practice. Might that being going on at St. Elizabeth's, too?)
It is too late to save Quincy Medical Center, but it is not too late for the state to review these matters and intervene.