Sunday, November 28, 2010
Behind the scenes
Friday, November 26, 2010
Painfully slow
What would prompt that? This New York Times article, citing a forthcoming NEJM study about medical errors in North Carolina. Here's the lede:
Efforts to make hospitals safer for patients are falling short, researchers report in the first large study in a decade to analyze harm from medical care and to track it over time.
The study, conducted from 2002 to 2007 in 10 North Carolina hospitals, found that harm to patients was common and that the number of incidents did not decrease over time. The most common problems were complications from procedures or drugs and hospital-acquired infections.
Other excerpts:Dr. Landrigan’s team focused on North Carolina because its hospitals, compared with those in most states, have been more involved in programs to improve patient safety.
But instead of improvements, the researchers found a high rate of problems.. . . The findings were a disappointment but not a surprise, Dr. Landrigan said. Many of the problems were caused by the hospitals’ failure to use measures that had been proved to avert mistakes and to prevent infections from devices like urinary catheters, ventilators and lines inserted into veins and arteries.
And another:
Dr. [Bob] Wachter said the study made clear the difficulty in improving patients’ safety.
“Process changes, like a new computer system or the use of a checklist, may help a bit,” he said, “but if they are not embedded in a system in which the providers are engaged in safety efforts, educated about how to identify safety hazards and fix them, and have a culture of strong communication and teamwork, progress may be painfully slow.”
Exactly right, Bob! What does it take to motivate this profession? What does it take to make process improvement part of medical school and residency training programs.Painfully slow, and painful or worse to patients.
---
Addendum: Dr. Wachter also discusses this study on his blog, here.
Tuesday, November 23, 2010
Things we are grateful for this year
The rally is timed to coincide with a weekend when most of us in the United States are celebrating Thanksgiving and are with the very people with whom we should be having these unbelievably important conversations – our closest friends and family.
At the heart of Engage With Grace are five questions designed to get the conversation about end-of-life started. We have included them at the end of this post. They are not easy questions, but they are important -- and believe it or not, most people find they actually enjoy discussing their answers with loved ones. The key is having the conversation before it’s too late.
This past year has done so much to support our mission to get more and more people talking about their end-of-life wishes. We’ve heard stories with happy endings … and stories with endings that could have (and should have) been better. We have stared down political opposition. We have supported each other’s efforts. And we have helped make this a topic of national importance.
So in the spirit of the upcoming Thanksgiving weekend, we’d like to highlight some things for which we’re grateful.
Thank you to Atul Gawande for writing such a fiercely intelligent and compelling piece on “letting go”– it is a work of art, and a must read.Thank you to whomever perpetuated the myth of “death panels” for putting a fine point on all the things we don’t stand for, and in the process, shining a light on the right we all have to live our lives with intent – right through to the end.
Thank you to TEDMED for letting us share our story and our vision.
And of course, thank you to everyone who has taken this topic so seriously, and to all who have done so much to spread the word, including sharing The One Slide.
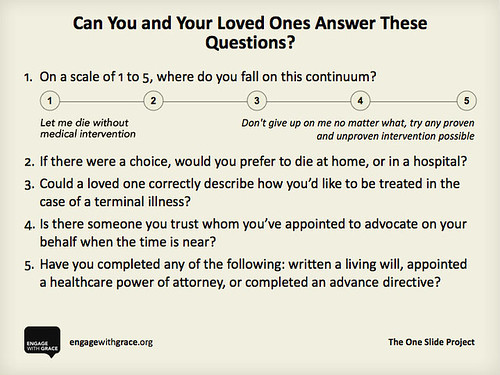
We share our thanks with you, and we ask that you share this slide with your family, friends, and followers. Know the answers for yourself, know the answers for your loved ones, and appoint an advocate who can make sure those wishes get honored – it’s something we think you’ll be thankful for when it matters most.
Here’s to a holiday filled with joy – and as we engage in conversation with the ones we love, we engage with grace.
To learn more please go to www.engagewithgrace.org. This post was written by Alexandra Drane and the Engage With Grace team. Please feel free to join our blog rally by copying this post and putting it on your own blog for this holiday weekend.Monday, November 22, 2010
Checklists ain't all
The emphasis on checklists is a Hitchcockian “McGuffan”, a distraction from the plot that diverts attention from how safer care is really achieved. Safer care is achieved when all three—not just one—of the following are realised: summarise and simplify what to do; measure and provide feedback on outcomes; and improve culture by building expectations of performance standards into work processes. We propose that widespread deployment of checklists without an appreciation of how or why they work is a potential threat to patients' safety and to high-quality care.
Sunday, November 21, 2010
Transparency and "dial tone" to fight market power
On the one hand, ACOs offer the potential for a better integration of care across the spectrum of primary care, hospitalization, skilled nursing, rehabilitation, and hospice. If the ACO faces an annual budget per patient under a capitated payment scheme, there is an incentive to avoid unnecessary tests and procedures and also to help direct patients to the most cost-effective component of the health care continuum.
On the other hand, if an ACO becomes the dominant provider in a region and especially if it has a electronic health record that is not interoperable with others in the region, that ACO will have substantial market power and will negotiate a higher global payment than would occur in a more competitive marketplace.
Robert Pear raises similar questions in an article in the New York Times. Here are some excerpts:
[E]ight months into the new law there is a growing frenzy of mergers involving hospitals, clinics and doctor groups eager to share costs and savings, and cash in on the incentives. They, in turn, have deployed a small army of lawyers and lobbyists trying to persuade the Obama administration to relax or waive a body of older laws intended to thwart health care monopolies. . . .
Attorney General Martha Coakley cautioned Friday against a "full-scale push forward" on global payment reform to address spiraling health care costs without addressing the underlying issue of market clout that has led to a disparity in pricing among providers without any clear link to quality of care.
. . . [S]he has directed her staff to resume its effort of examining the health care market in Massachusetts to study models of care delivery and the associated costs.
. . ."A shift to global payments by itself is not the panacea to controlling costs," Coakley said. "Implementing payment reform without addressing the market leverage issue outlined in our report is like trying to fix the roof on a house without fixing the flawed foundation."
Because anti-trust regulatory action is often ineffective against market dominance, we should focus on self-reinforcing policy initiatives to mitigate against this possibility. Here are two suggestions.
The first is one mentioned often on these pages: Total transparency of rates paid by each insurance company to each provider. In Masachusetts, a good first step along these lines was taken by the Legislature and Governor Patrick this past summer. Only when subscribers can see the actual rates being paid will there be the moral force to ensure that rates are reasonably related to factors other than market power.
The second idea is a simple as dial tone: Complete interoperability of medical records among providers. As long as proprietary electronic medical record systems exist, a given provider network can control the degree to which patients can choose lower priced or higher quality doctors and hospitals outside of that network.
Instead, we need the equivalent of the "magic button" described in this post by our CIO, John Halamka, demonstrating interoperability between our hospital and Atrius, the state's largest multi-specialty practice:
By working with Epic and Atrius, we enabled a "Magic Button" inside Epic that automatically matches the patient and logs into BIDMC web-based viewers, so that all Atrius clinicians have one click access to the BIDMC records of Atrius patients.
If this capability existed among and between all provider systems, consumer choice would be possible. Without it, a dominant network will remain dominant.
Saturday, November 20, 2010
A defining moment at Risky Business

 Lord Ian Blair led London's Metropolitan Police through the investigations of the multiple bombings of July 7, 2005 and all that followed. His lessons about chain of command and the like are valuable to those who have to deal with disasters and emergencies. He presented this at the Risky Business conference in London this week.
Lord Ian Blair led London's Metropolitan Police through the investigations of the multiple bombings of July 7, 2005 and all that followed. His lessons about chain of command and the like are valuable to those who have to deal with disasters and emergencies. He presented this at the Risky Business conference in London this week.If you cannot view the video, click here.
BP Oil Spill at Risky Business
 Here is a very good perspective on what went wrong to cause the explosion on the BP Deepwater Horizon drilling rig and the resultant oil spill, presented by Nick Coleman, VP in charge of Group Safety Performance Reporting until three years before the incident. He is now non-executive chair of the Risk and Safety Committee of Royal Brompton Hospital. He presented this at the Risky Business conference in London this week.
Here is a very good perspective on what went wrong to cause the explosion on the BP Deepwater Horizon drilling rig and the resultant oil spill, presented by Nick Coleman, VP in charge of Group Safety Performance Reporting until three years before the incident. He is now non-executive chair of the Risk and Safety Committee of Royal Brompton Hospital. He presented this at the Risky Business conference in London this week.If you cannot view the video, click here.
Everest disaster at Risky Business
 Dr. Ken Kamler is a surgeon who also has served as doctor on some of the world's most daring expeditions, including the ill-fated climb up Mt. Everest in 1996. He told that story in this presentation at Risky Business in London this week.
Dr. Ken Kamler is a surgeon who also has served as doctor on some of the world's most daring expeditions, including the ill-fated climb up Mt. Everest in 1996. He told that story in this presentation at Risky Business in London this week.If you cannot see the video, click here.
Reconciliation at Risky Business
 Jo Berry is founder of a charity called Building Bridges for Peace. Patrick Magee, PhD, was sentenced to life imprisonment for the Brighton Bomb which he set off as a member of the Provisional Irish Republican Army in 1984. He was released in 1999. For 10 years he has worked for peace with Jo Berry, whose father he killed at Brighton.
Jo Berry is founder of a charity called Building Bridges for Peace. Patrick Magee, PhD, was sentenced to life imprisonment for the Brighton Bomb which he set off as a member of the Provisional Irish Republican Army in 1984. He was released in 1999. For 10 years he has worked for peace with Jo Berry, whose father he killed at Brighton.They offered this discussion at Risky Business in London yesterday.
If you cannot see the vido, click here.
Friday, November 19, 2010
Sekou at Risky Business
if you can't see the video, click here.
Pedro Algorta at Risky Business
If you can't see the video, click here.
Thursday, November 18, 2010
Risky decision-making
The aim of this conference is to hear from some of the highest achievers in other high risk industries on the topics of risk, human factors, patient safety, teamwork, leadership, and improvement.
The presentations have been among the best I have heard anywhere. There are several I would summarize, but for now, please consider watching this one by Pat Croskerry, Professor in Emergency Medicine at Dalhousie University, Halifax, Nova Scotia.
Croskerry's exposition compares intuitive versus rational (or analytic) decision-making. Intuitive decision-making is used more often. It is fast, compelling, requires minimal cognitive effort, addictive, and mainly serves us well. It can also be catastrophic in that it leads to diagnostic anchoring that is not based on true underlying factors.
Why is it addictive? Croskerry describes the "cognitive miser function," a tendency to get comfortable with the form of decision-making that you find most used and useful.
The problem, of course, is that the overall rate of diagnostic failure is about 15%, and most of those diagnoses are made based on the intuitive approach. Not that the analytic approach is always correct, either. Indeed, in studies of factors contributing to failures to diagnose, cognitive errors alone or in part account for about 75% of the cases.
Croskerry thinks we need to spend more time teaching clinicians to be more aware of the importance of decision-making as a discipline. He feels we should train people about the various forms of cognitive bias, and also affective bias. Given the extent to which intuitive decision-making will continue to be used, let's recognize that and improve our ability to carry out that approach by improving feedback, imposing circuit breakers, acknowledging the role of emotions, and the like.
While you are at it, check out the video of this presentation by Duncan Murrell, who employs intuitive decision-making while photographing humpback whales -- sometimes in the middle of a feeding frenzy -- from a kayak in Southeast Alaska. (You can see the photographs up close here.)
If you can't see the videos, click here.
MLB praises Red Sox Scholars program
Major League Baseball announced today that the Boston Red Sox have been named the recipient of the inaugural Commissioner's Award for Philanthropic Excellence. Created by Major League Baseball and chosen by a Blue Ribbon Panel comprised of Commissioner Allan H. (Bud) Selig and MLB Executives, the award recognizes the Red Sox extraordinary charitable programs, run by the Red Sox Foundation, which have resulted in significant and sustained community impact.
Commissioner Selig presented the club with the award today at the Industry Meetings in Orlando, FL. . . .In singling out the Red Sox for this prestigious award, the Commissioner praised the depth of the Red Sox charitable programs and specifically the impact of the Red Sox Scholars program, the educational cornerstone of the Red Sox Foundation.
... said Commissioner Selig. "I congratulate the entire Boston Red Sox organization, and particularly the Red Sox Foundation, for their commitment to the future of hundreds of young people from the inner-cities of Boston."
... Each year, the Red Sox select 25 academically talented, economically disadvantaged Boston Public School students in 5th grade as Red Sox Scholars. Through the program, run by the Red Sox Foundation, the Scholars receive tutoring, mentoring, after school enrichment opportunities, summer camp assistance, and other leadership development activities. Red Sox Foundation staff members work with the Scholars intensively in 6th through 12th grades and each Scholar is awarded a $10,000 college scholarship redeemable upon graduation from high school with enrollment in an accredited college, and on condition of continued good citizenship. There are currently 200 Red Sox Scholars with members of the first class selected in 2003 now college freshmen.
The Red Sox Scholars program is presented by Beth Israel Deaconess Medical Center (BIDMC), the Official Hospital of the Boston Red Sox. Over the years, almost 200 BIDMC physicians, nurses, medical technicians and administrators have been individually paired with the Scholars as Medical Champions. BIDMC also hosts "Shadow Days" for the Scholars each year, giving them an opportunity to visit the Neo-natal Intensive Care Unit, the Simulation Center and Skills Lab, and other parts of the medical center to be exposed to a variety of careers in medicine.
Wednesday, November 17, 2010
ED report card
Here is the trend in our place. Each year we admit about a dozen residents. Note the growth in applicants year to year in the top chart.
And the chart underneath shows their performance on the standardized examination. Nicely above average year after year for all three classes of residents.
Tuesday, November 16, 2010
The US dialysis program -- How good and how bad?
A recent article in ProPublica by Robin Fields contains a number of strong criticisms of the US dialysis program for people with kidney disease. Here's an excerpt:
Now, almost four decades later, a program once envisioned as a model for a national health care system has evolved into a hulking monster. Taxpayers spend more than $20 billion a year to care for those on dialysis -- about $77,000 per patient, more, by some accounts, than any other nation. Yet the United States continues to have one of the industrialized world's highest mortality rates for dialysis care. Even taking into account differences in patient characteristics, studies suggest that if our system performed as well as Italy's, or France's, or Japan's, thousands fewer patients would die each year.
NPR's Terry Gross recently interviewed both Robin Fields and Barry Straube, Chief Medical Officer for Medicare. The interviews are worth hearing or reading. Here's an excerpt from Dr. Straube's interview:
I believe that Robin's article, although pointing up some very important issues that this agency and the Department of Health and Human Services is aware of and trying its best to fix, that it overstates significantly the degree of the problem out in the real world. It makes it sound like any dialysis unit that a patient would walk into is subject to these problems and that's simply not true. The vast, vast majority of the units are not as described in the several examples, which are completely true examples but not illustrative of most dialysis units.
I think my main quibble with the article is that it sounds as though one would not want to have dialysis in the United States. This is a life-saving treatment that the vast majority of people are being treated very well in very clean facilities that hopefully make very few mistakes. And the examples there are not indicative of most dialysis units.
I conclude, having read and heard both, that there are elements of truth in the article about this kind of care and need for improvement. However, the magnitude of the problem seems to me to be less than reported. I welcome your thoughts.
Monday, November 15, 2010
Middle school explorers in BIDMC Labs
Four students from the William Barton Rogers Middle School in Hyde Park spent a morning at BIDMC with Parameswary Muniandy, PhD, a pathology research fellow studying brain cancer. “Early exposure to science and how research works really helps them develop an interest in science,” said Muniandy. She helped the students feel like real researchers by putting on lab coats and gloves.
You can watch the excitement in this video. If you can't see the video, click here.
Some grades are in
 In a comment below, Jim Conway offers some data from the Commonwealth Fund that sheds light on the question posed. I have copied the summary above.
In a comment below, Jim Conway offers some data from the Commonwealth Fund that sheds light on the question posed. I have copied the summary above.Recall that the proposition was: "There is lots of evidence that Massachusetts health care is the best in the country." We get excellent grades for access and equity. This is not surprising given the state's universal insurance coverage law.
We do well on "healthy lives," too, but I do not know how much of that derives from the health care system as opposed to relative lifestyle (smoking, obesity, and the like) in the Bay State.
But we clearly have a problem when it comes to overuse of the hospital system. Also, the performance with regard to standard indicators of care is not exemplary.
Sunday, November 14, 2010
Prove it!
I was taken aback. I have never seen any evidence to support this conclusion. Would anyone care to offer quantitative support for the proposition -- or against it?
A mission to a tiny country
The goal of this mission is to do an initial assessment of the need for urological specialty care, while diagnosing and possibly treating a number of patients while there. The team believes they will be seeing approximately 100 patients over 4 days.
But what I really like, too, is that our Interpreter Services Department offered to join in, selflessly concluding that this would be a great opportunity to assist in the development of this service.
In all, three BIDMC Cape Verdean interpreters, two Chief Residents from BIDMC, and one doctor from the Miriam Hospital, are joining Dr. Kearney on this mission.
Through the generosity of the Cape Verdean consulate in Boston, TACV airlines, the clinics in Cape Verde to be visited, and Nobidade TV media, expenses for travel will be kept to a minimum.
Please join me in wishing them all well.
Saturday, November 13, 2010
Rolling Thunder
Newton Girls Soccer team Thunder ended the fall season with a triumphant 7-1-2 record, clinching the championship of their section of under-14 players. Congratulations to all!


